|
<< Click to Display Table of Contents >> Description and Usage |
  
|
|
<< Click to Display Table of Contents >> Description and Usage |
  
|
The Insurance Billing Time Analysis Report provides the number of days between the Discharge Date and the Medical Record Finish Date, the Admission Date and the date the approval was sent, the Approval Sent Date and the Approval Received Date, the Discharge Date and the date the claim was generated, the generation date and the date the claim was billed, the Billed Date and the date payment was received, and the Discharge Date and Payment Received Date. The report will sub-total by Financial Class Code, and provide averages for each column.
Insurance Billing Time Analysis
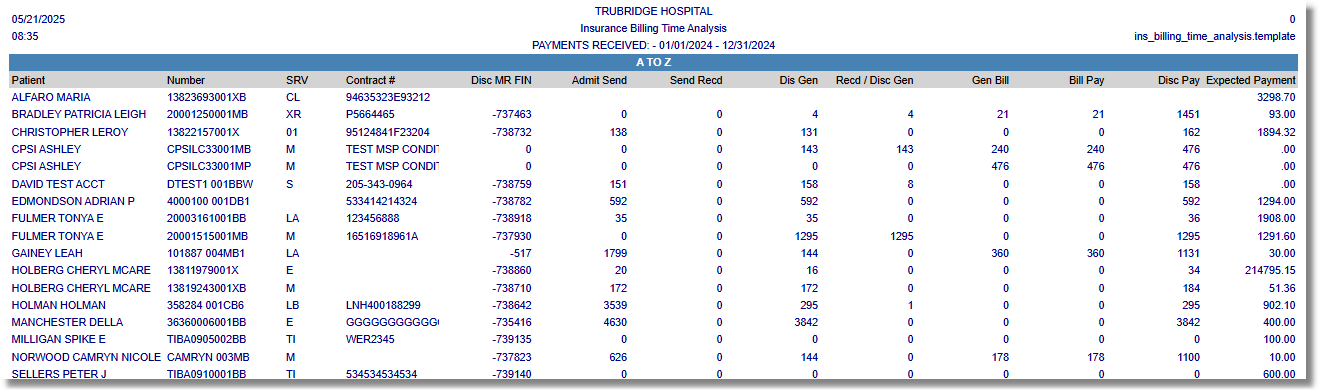
Listed below is an explanation of each column.
•Patient: Pulls from the Full Name field on the Patient tab within the Registration and ADT screen.
•Number: Pulls the Patient Control Number from the Claims Status screen.
•Srv (Service Code): Pulls from the Patient tab within the Registration and ADT screen.
•Contract #: Pulls from Policy Information screen.
•Disc MR Fin: The number of days between the Discharge Date and the Medical Record Finish Date.
•Admit Sent: The number of days between the Admission Date and the date the approval was sent.
•Send Recd: The number of days between the Approval Sent Date and the Approval Received Date.
•Disc Gen: The number of days between the Discharge Date and date the claim was generated.
•Recv/Dis Gen: If the Approval has not been received before the Discharge Date, then this is number of days between the Approval Received Date and the date of generation. If Approval has been received before the Discharge Date, then this is the number of days between the Discharge Date and the date of generation.
•Gen Bill: The number of days between the Generation Date and the date the claim was billed.
•Bill Pay: The number of days between the Billed Date and Payment Received Date.
•Disc Pay: The number of days between the Discharge Date and Payment Received Date.
•Expected Payment: The Expected Pay amount pulls from the Detail Charges screen.