|
<< Click to Display Table of Contents >> Assessment |
  
|
|
<< Click to Display Table of Contents >> Assessment |
  
|
The Assessment section of the Patient Medical Summaries is an overall evaluation of the patient visit. "No Data Found" will display if no information is entered for the section.
Select Patient Account > Health History > New > Referral/Transition of Care > Patient Medical Summaries > Patient Summary 2.1.4 > Assessment
Assessment
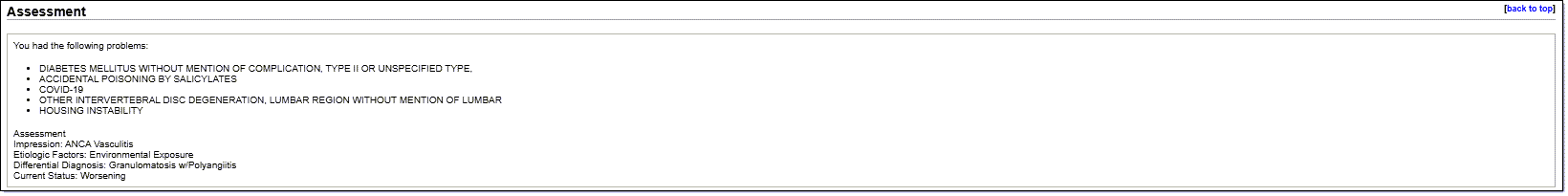
The Assessment section of the CCDA includes:
•Active problems entered or documented against, in the Problem List.
•On inpatients the Assessment section consists of the last signed Progress Note.
•On patients in the EDIS department or TPEHR clinic, the Assessment section contains all documentation entered on the Assessment section of a document within the Documentation application. This includes the predefined information within the document, and information added from Charting Options or Quick Add text boxes. Information retracted or amended will not be included.
•On patients with a signed Note that includes the Patient Medical Summaries filter Assessment, any documentation within the Assessment filter will display.