|
<< Click to Display Table of Contents >> Detail Charges |
  
|
|
<< Click to Display Table of Contents >> Detail Charges |
  
|
This option contains information from the patient's Account Detail. There are two Detail Charges screens that are used within the system. One is an itemized screen usually used for Outpatient claims. The other is a summarized screen for Inpatient claims.
Select Web Client > System Menu > Hospital Base Menu > Patient Account # > Insurance > Claim > Itemized Detail Charges
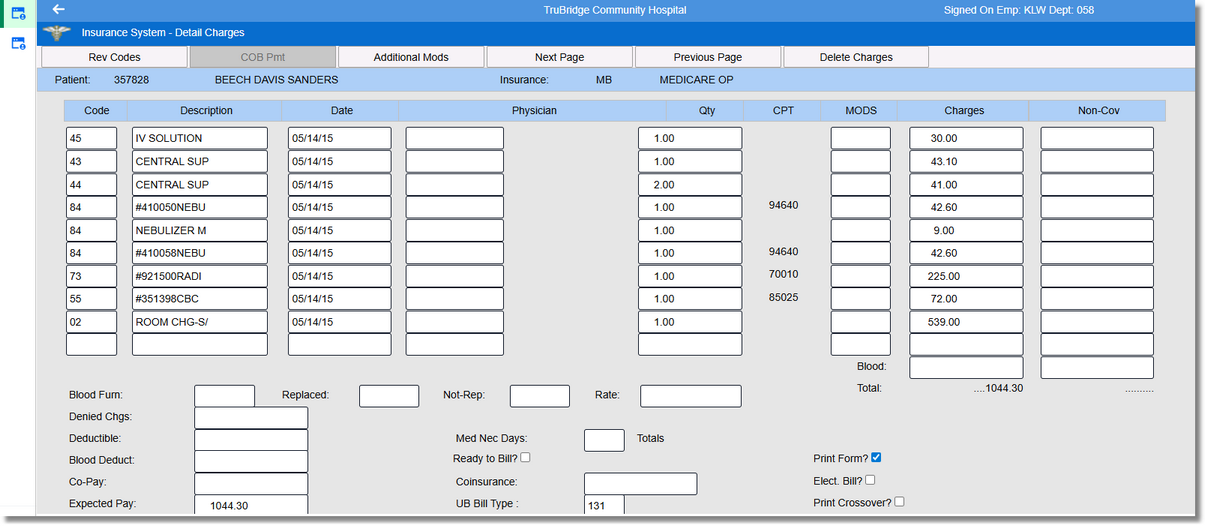
Insurance System - Detail Charges
Select Web Client > System Menu > Hospital Base Menu > Patient Account # > Insurance > Select Claim > Summarized Detail Charges
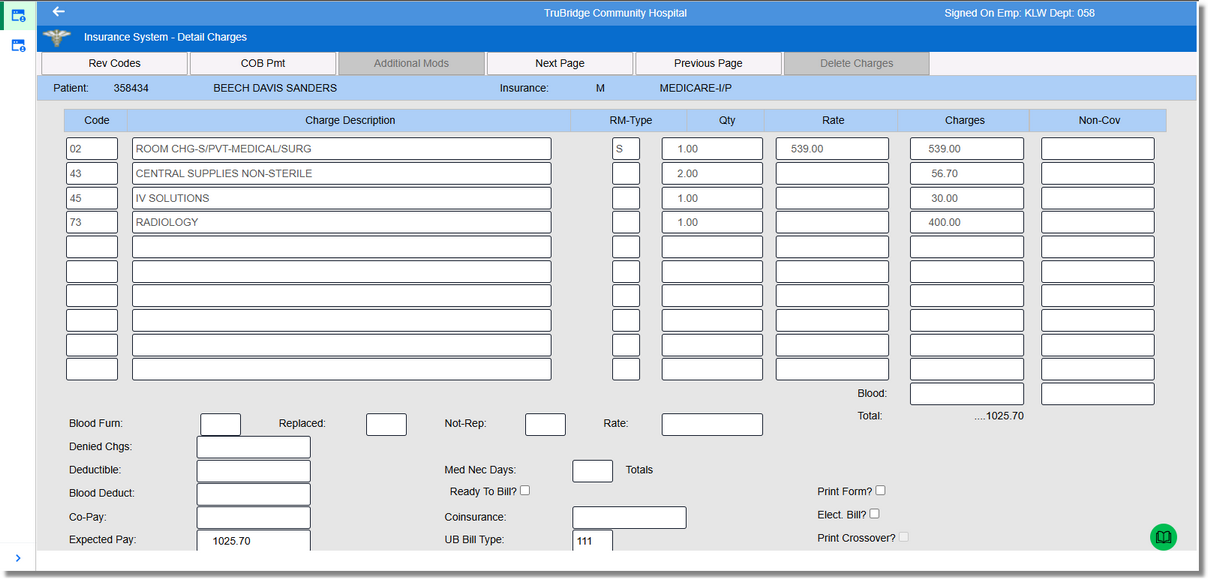
Insurance System - Detail Charges
The majority of this screen is used to display the charges that will pull to a claim. Once a claim is generated, the charges within the date range selected will pull to the Detail Charges screen from the Account Detail. Charges may be manipulated on this screen without affecting the patient’s Account Detail.
Outpatient claims pull an itemized Detail Charges screen. The Outpatient information pulls the Summary Code from the Item Master. The Charge Description looks to the Item Master at the time the charge is posted to the account to pull the Item Description. If the item has a CPT Code loaded on the Item Master Maintenance screen, the description will pull with "#" and the item number preceding the Summary Code description. If the item does not have a CPT Code loaded on the Item Master, the description from the Summary Code Table will pull to the Detail Charges screen. The date the charge was incurred also pulls to these fields. The Physician name and number, based on what was entered during charging, pulls to these fields on the itemized Detail Charges screen. The quantity pulls from the Account Detail and is the amount that was entered during charging. The rate is calculated by taking the total charges from the Account Detail and dividing it by the quantity. CPT Modifiers pull from the Item Master Maintenance. The Modifiers are the last four characters in the 9-character CPT Code. The covered and non-covered charge amounts are the same for itemized screens and summarized screens.
Inpatient claims pull a summarized Detail Charges screen. Like an Outpatient claim, the charges pull from the Account Detail. The charges pull the 2-character Summary Code that is associated with the charge in the Item Master. This pulls to the Account Detail at the time the charge is posted. The charge description pulls from the Account Detail that pulled from the description of the Summary Code at the time the charge was posted. Room Type is only used for room charges and pulls the type of room from the Census charges. The Quantity also pulls from the Account Detail. This is entered during the charging process. The Rate is the dollar amount charged for a single item. The system takes the total amount charged from Account Detail and divides it by the Quantity to get the rate. The Covered Charges are a total amount of charges less the Non-Covered Charges. Non-Covered Charges show on an account if the Room Rate is higher than the amount on the Detail Benefits screen. These Non-Covered Charges also show if the Coverage Percentage is less than 100 on the Detail Benefits screen. Not entering the Full Days on the Detail Benefits screen for Inpatient accounts also results in charges being non-covered.
NOTE: If the Contract Billing Report was used to transfer specific charges from a patient's account to a master account, only the charges that are not transferred will be included on the patient's insurance claim.
The following fields are on the Detail Charges screen for both itemized and summarized claims:
•Blood: The blood charges from the patient account will pull to this field.
•Blood Furn: Replaced: Not Rep: Rate: These fields require the information to be loaded manually. The Blood Furnished field stores the number of pints of blood furnished for the patient. Replaced is the field that stores the information on the number of pints of blood replaced. The number of pints of blood not replaced is loaded in the Not-Rep field. The Rate field is the average rate of each pint of blood.
•Denied Chgs: The Denied Charges field stores the dollar amount of the charges that the insurance company refused to pay. This field is updated manually and will reduce the Expected Pay for the claim.
•Deductible: The Deductible amount pulls the dollar amount that was loaded on the Detail Benefits screen. This field is also updated during the receipting process.
•Blood Deduct: The Blood Deductible should be entered manually.
•Co-Pay: This field may be updated at any time during the insurance billing process. When adjusting this field, the Expected Pay field will reflect the adjustment.
•Expected Pay: The Expected Pay field is calculated each time the claim is generated. The system takes the total charges for the claim less the Non-Covered, Deductible, Co-pay, Coinsurance and Denied Charges to compute the Expected Pay. This pulls to locator 55 on the UB.
•Med Nec Days: Medically Necessary Days should be entered manually.
•Ready to Bill?: This field defaults to No. When the claim has been through the billing process and is ready to bill, this field should be selected.
•Coinsurance: This field may be updated at any time during the insurance billing process. When adjusting this field, the Expected Pay field will reflect the adjustment.
•UB Bill Type: This field is computed by the system for Bill Types 111 - 114, 131 - 132, 831 and 851. Other Bill Types needed may be entered on page 1 of the Insurance Companies Table. This field's information may be over keyed at any time. This pulls to locator 4 on the UB.
•Print Form?: The Print Form field should be answered when the claim is Ready to Bill. Selecting this field will allow the claim to print on a form, and leaving the field blank will suppress the claim from printing. Although the claim will not print, the system will still advance the claim status. For more information on this field, see Stages of an Insurance Claim section of this User Guide.
•Elec Bill?: This option is allowed on claims that have the Transmit Claim field on page 1 of the Insurance Companies Table set Y. This will allow the claim to pull to the electronic file for this Financial Class. For more information on this field see Insurance Tickler.
•Print Crossover?: This field should be answered Y if a crossover form will be printed for the claim.
The following options are located at the top of the screen:
•Rev Codes: This option will toggle back and forth from the Summary Code display to the Revenue Code display. Selecting Rev Codes will display the Revenue Code on the Detail Charges screen. Selecting Sum Codes will display the Summary Codes.
•COB Prnt: This option is state specific for Michigan.
•Additional Modifiers: This option will allow Additional Modifiers to be added to those already listed in the Detail Charges screen.
Select Web Client > System Menu > Hospital Base Menu > Patient Account # > Insurance > Select Claim > Detail Charges > Additional Modifiers
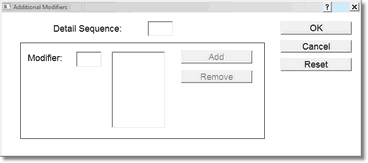
Insurance System - Additional Modifiers
Selecting the Additional Modifiers option will prompt for the Detail Sequence. Enter the number of the Detail Charge line that corresponds to the line in which the Modifier should be added; (ie. If the Modifier should be added to the third line down in the Detail Charges screen, enter a 3 in the box.) Select OK once the sequence number is entered. Enter the Modifier to be added and select Tab on the keyboard to move to the Add option. Selecting Add will display the Modifier.
Once all information has been entered, select OK to complete the addition of the Modifier. The Reset option may be selected if the information entered was incorrect and needs to be cleared. After a Modifier has been added it can be removed by entering the Detail Sequence number of the line, highlighting the incorrect Modifier, then selecting the Remove option. Additional Modifiers will pull to locator 44 of the UB and locator 24D of the 1500.
•Next Page: Previous Page: Select either option to view more or toggle back to prior charges on the Detail Charges screen.
•Delete Charges: This option will delete all charges on the page.
•Anesthesia: This view only option will display if there are anesthesia charges that have been generated on the claim. See Anesthesia Charging and Billing in Additional Documentation for more information.