|
<< Click to Display Table of Contents >> Description and Usage |
  
|
|
<< Click to Display Table of Contents >> Description and Usage |
  
|
The Account Reconciliation Screen will display activity for accounts with a current balance. The account activity is grouped by month and will include the following: charges, adjustment charges, patient payments, insurance charges, insurance payments, contractual amounts and monthly payments. The information may be viewed for a specific account, or a list may be created using a range of admit dates, discharge dates or activity dates. Once the information is displayed on the screen, PDF may be selected to display the results in a PDF format, or CSV may be selected to display the results in an CSV format.
Account Reconciliation Screen
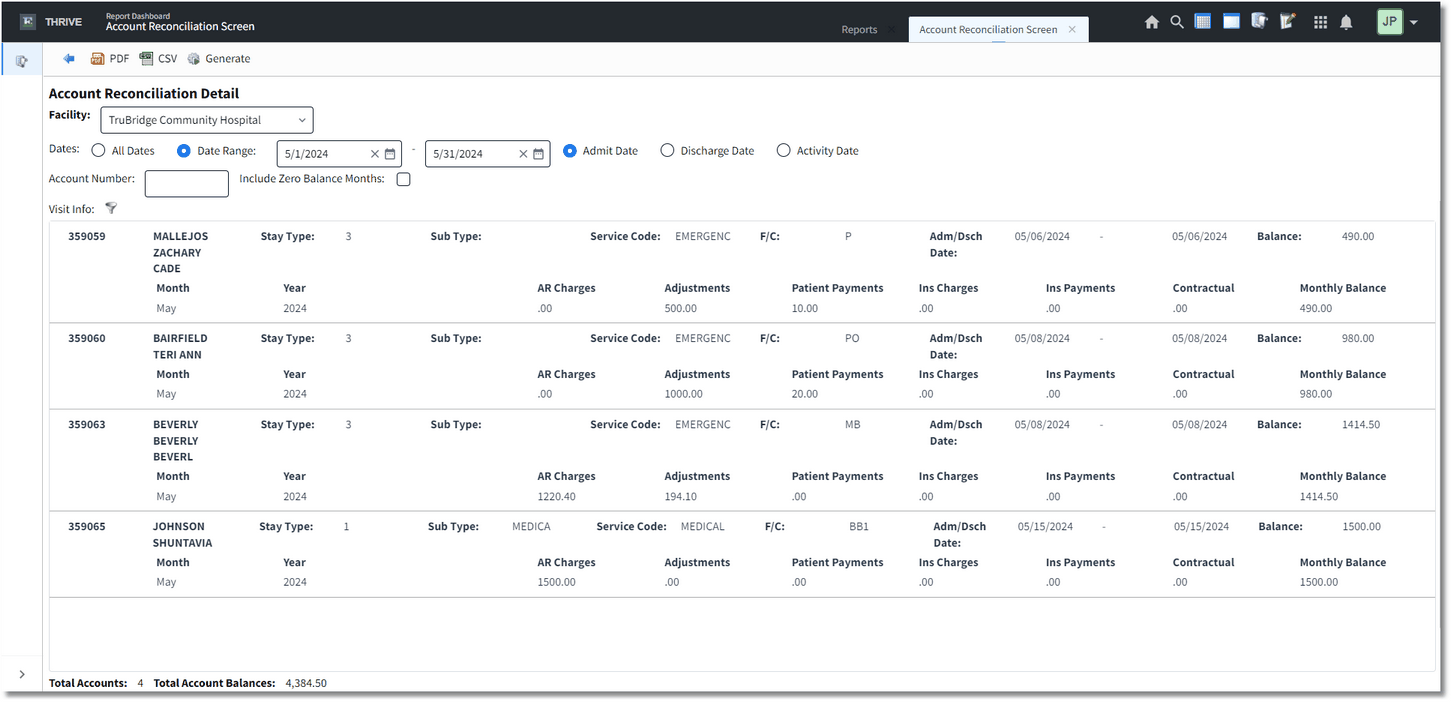
Listed below is an explanation of each column.
•Account: Pulls the patient account number and patient name from the Registration and ADT screen.
•Stay Type: Pulls from the Patient tab on the Registration and ADT screen.
•Sub Type: Pulls from the Patient tab on the Registration and ADT screen.
•Service Code: Pulls from the Patient tab on the Registration and ADT screen.
•F/C: Pulls the financial class from the Guarantor/Insurance tab on the Registration and ADT screen.
•Adm/Dsch Date: Pulls the Admit and Discharge dates from the Stay tab on the Registration and ADT screen.
•Balance: The total outstanding account balance.
•Month: The month for which the activity is being reported.
•Year: the year for which the activity is being reported.
•AR Charges: The total AR charges on the account for the selected time period.
•Adjustments: The total adjustment charges on the account for the selected time period.
•Patient Payments: The amount paid by the patient. If the receipt is entered with a service date present, the receipt will reflect in the month of the service date. If there is no service date present, the receipt will reflect in the month of its AR date.
•Ins Charges: The total charges billed on the insurance claim for that time period. This will include any claims that are at the Ready to Bill, Unchecked, Billed and Pending status.
•Ins Payments: The amount paid by insurance. This will use the patient's insurance claims' service dates to determine in which month the payment will be reported.
•Contractual: The insurance contractual amount.
•Monthly Balance: The outstanding account balance for the month selected.
Totals
•Total Accounts: The total number of patient accounts that pulled within the selected date range.
•Total Account Balances: The total dollar amount of the patient accounts that pulled for the selected parameters.