|
<< Click to Display Table of Contents >> Checking Eligibility |
  
|
|
<< Click to Display Table of Contents >> Checking Eligibility |
  
|
Once all configurations have been completed, select Check Eligibility within the patient's expanded demographics to launch the Check Eligibility screen. Keep in mind, this option will only be enabled if there is a visit AND insurance claim linked to the appointment.
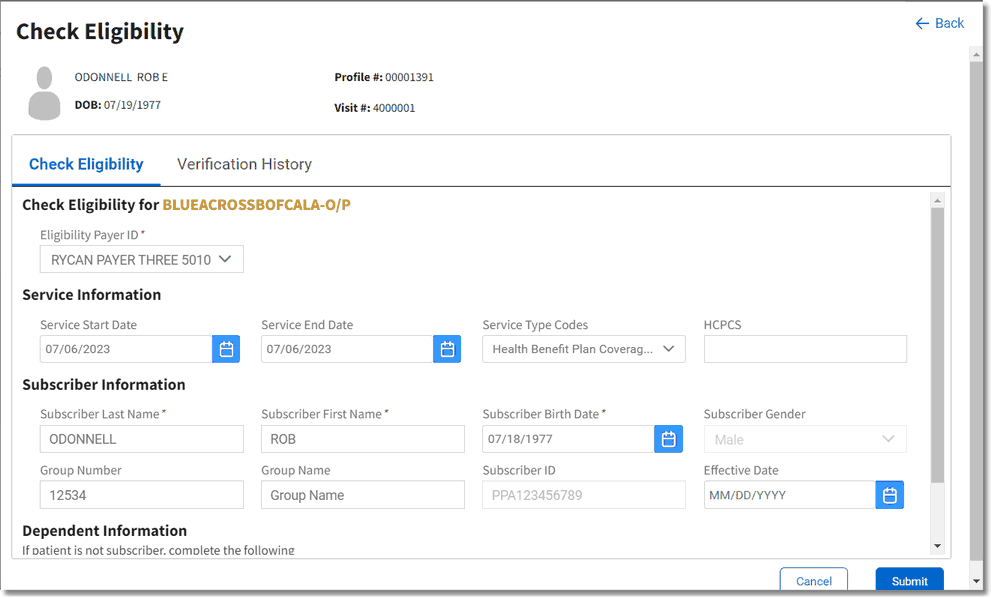
Check Eligibility
Once the Check Eligibility screen displays, the following options may be addressed:
•Eligibility Payer ID: This drop-down will automatically display the TruBridge RCM payer identifier in the Insurance Companies table, if present. If a Payer ID does not display, select the drop-down to select the appropriate Payer ID.
NOTE: The Payer ID drop-down may be selected to override any automated selection in the event a different value is needed.
Service Information
•Service Start/End Date: These fields will default to the date of the appointment.
•Service Type Codes: This drop-down will default to the values specified in the Configurations screen; however, this may be modified by selecting or deselecting various service type codes.
•HCPCS: Up to five procedure codes may be entered in this field. This is a free text field as there is no search option.
Subscriber Information
The information in this section pulls from the claim coverage in TruBridge EHR. The information in these fields may be edited and any changes will copy back to TruBridge EHR.
Dependent Information
The information in this section will automatically populate when applicable and may also be edited.
Once all information has been addressed, select Submit to start the eligibility check. The full 271 response, plus the option to request deductible, co-insurance, or co-payment amounts for the service being provided will display.
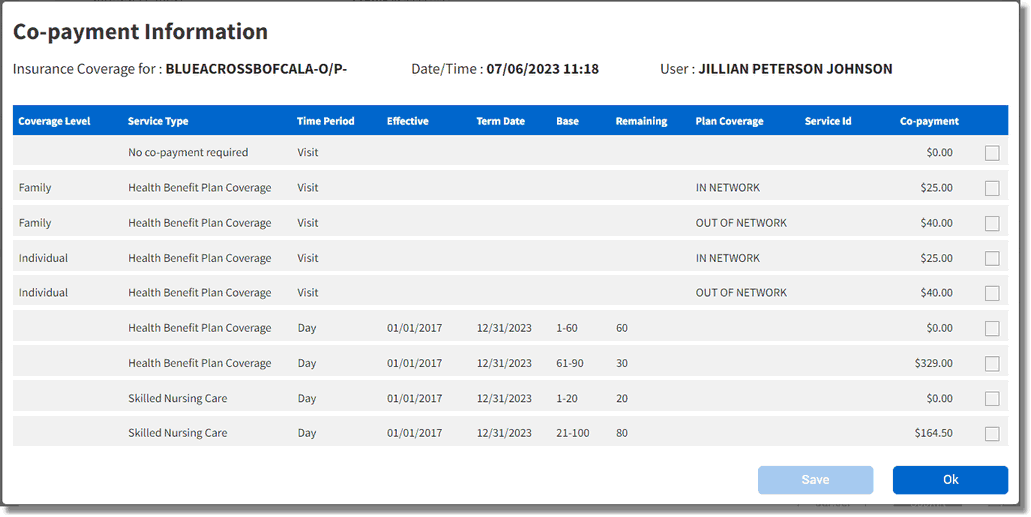
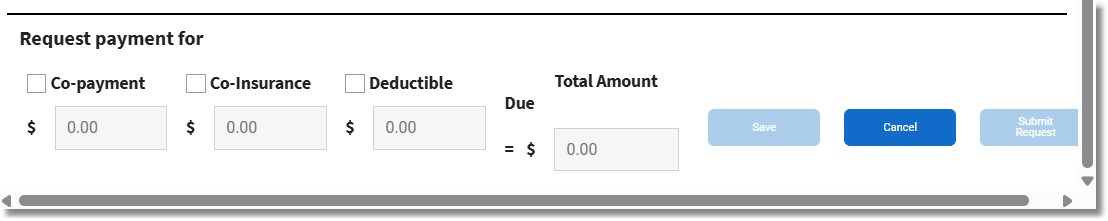
Payment Request Information
The Payment Request screen allows requests for a payment amount to be sent to the patient, even if the eligibility wasn't successful.
When a payment request is made, a message will be sent to the patient that specifies what the payment represents (deductible, co-insurance, or co-payment).
To request payment, select all applicable Request Payment for options (deductible, co-insurance, and/or co-payment). Then, enter the amount in the fields below each payment type. As amounts are entered, the total will be calculated and display in the Total Amount Due field. Select Submit Request to send the payment request to the patient. The payment type and amount will be displayed in the patient’s expanded demographics under Insurance Information with "Pending Receipt" below the amount.
If a payment type isn’t selected when eligibility is initially selected because more research is needed, select Save. A payment request may be sent later by re-launching the Check Eligibility screen and selecting the Verification History tab.